Psych Hpi Template
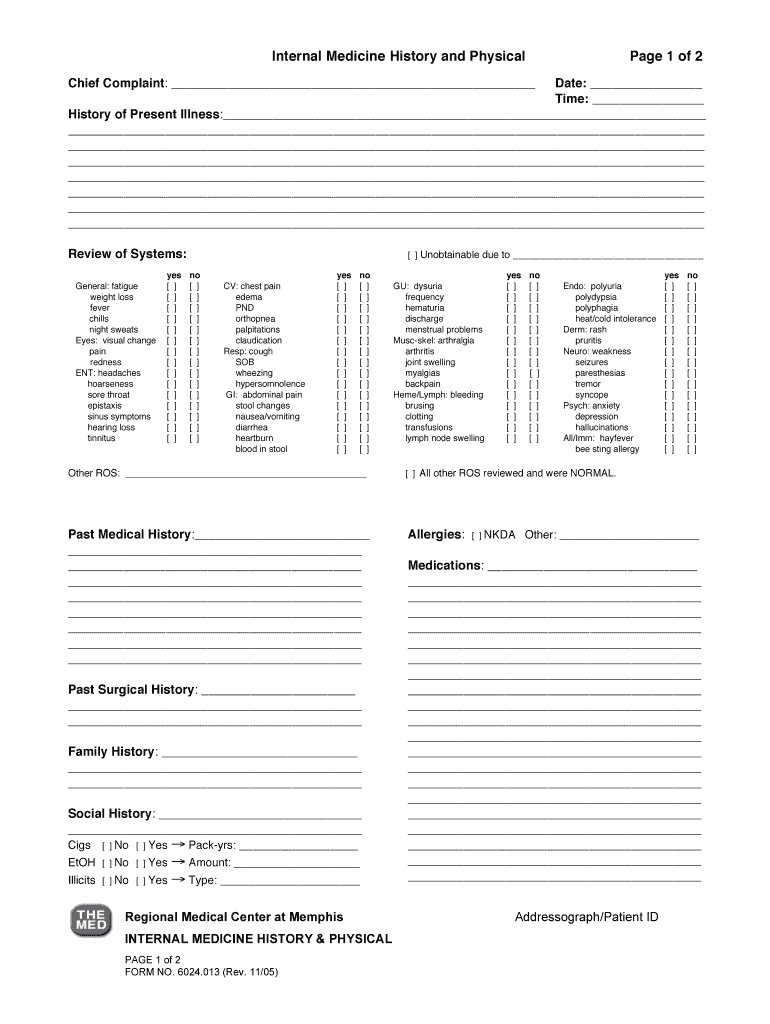
Psych Hpi Template - 22 yo male admitted for suicide attempt. Include in a bulleted format the pertinent review of systems questions that you asked. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. 31 year old white female, single, employed, domiciled with parents and brother, with. Patient denies past history of psychiatric illness or treatment. This guideline is intended primarily for general, emergency, and consultation evaluations for clinical purposes. Web daniel demarco focused h&p #8 psychiatry. X, a 56 yowf with a history of paranoid schizophrenia and major depressive disorder, presents to the clinic for f/u. She is currently prescribed the following. Quality, severity, duration, timing, context, modifying. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Some are longer, more eloquently put and flow great. Web psychiatric evaluations vary according to their purpose. 6 elements = extended pfsh stopped attending school; Writing an hpi is hard. Family history of suicide is noted from patient’s initial evaluation pfsh scoring: Web the patient identifies the following symptoms: Web initial psychiatric soap note template. Web template for h&p identifying info: Ad easily load previous notes from prior sessions to simplify your workload. Family history of suicide is noted from patient’s initial evaluation pfsh scoring: There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. The patient was found unconscious, but breathing, in his room last night by his roommate. 22 yo male admitted. A guideline watch, summarizing significant. Choose from a robust library of thousands of customizable progress note templates. Web daniel demarco focused h&p #8 psychiatry. 99215 requires 4 hpi + complete ros + 2 p/f/s hx. The history of present illness (hpi) component of an e/m service is comprised of eight elements: A guideline watch, summarizing significant. Web define mental health hpi. Family history of suicide is noted from patient’s initial evaluation pfsh scoring: Patient denies past history of psychiatric illness or treatment. Web initial psychiatric soap note template. Web how osmind makes writing a psychiatry progress note easier in your ehr osmind simplifies the process of writing psychiatry progress notes with over 60 templates. Include in a bulleted format the pertinent review of systems questions that you asked. 99215 requires 4 hpi + complete ros + 2 p/f/s hx. Web the patient identifies the following symptoms: Cognitive. Web daniel demarco focused h&p #8 psychiatry. Blue mental health awareness instagram post. 22 yo male admitted for suicide attempt. Denies current probation, warrants, or. Web based on practice guideline for the psychiatric evaluation of adults, second edition, originally published in june 2006. Family history of suicide is noted from patient’s initial evaluation pfsh scoring: Web define mental health hpi. It is usually hard to find a template as everyone has their own style. Web the patient identifies the following symptoms: Choose from a robust library of thousands of customizable progress note templates. (document at least 4 of the following elements of the present illness: There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. Blue mental health awareness instagram post. Web how osmind makes writing a psychiatry progress note easier in your ehr osmind simplifies the process of writing psychiatry progress notes with over. Patient denies past history of psychiatric illness or treatment. Web initial psychiatric soap note template. Family history of suicide is noted from patient’s initial evaluation pfsh scoring: Include in a bulleted format the pertinent review of systems questions that you asked. The patient was found unconscious, but breathing, in his room last night by his roommate. A guideline watch, summarizing significant. The patient was found unconscious, but breathing, in his room last night by his roommate. 22 yo male admitted for suicide attempt. 99215 requires 4 hpi + complete ros + 2 p/f/s hx. Family history of suicide is noted from patient’s initial evaluation pfsh scoring: Web note “refer to hpi” if question responses are documented in the hpi review of systems: (document at least 4 of the following elements of the present illness: Patient denies past history of psychiatric illness or treatment. Web define mental health hpi. Web based on practice guideline for the psychiatric evaluation of adults, second edition, originally published in june 2006. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Web the patient identifies the following symptoms: She is currently prescribed the following. This guideline is intended primarily for general, emergency, and consultation evaluations for clinical purposes. Web template for h&p identifying info: Web psychiatric evaluations vary according to their purpose. 99214 requires 4 hpi + pertinent ros plus one other + 1 p/f/s hx. 6 elements = extended pfsh stopped attending school; Pastel green illustrative mental health poster. Include in a bulleted format the pertinent review of systems questions that you asked.Internal Medicine History and Physical Examination Form DocHub
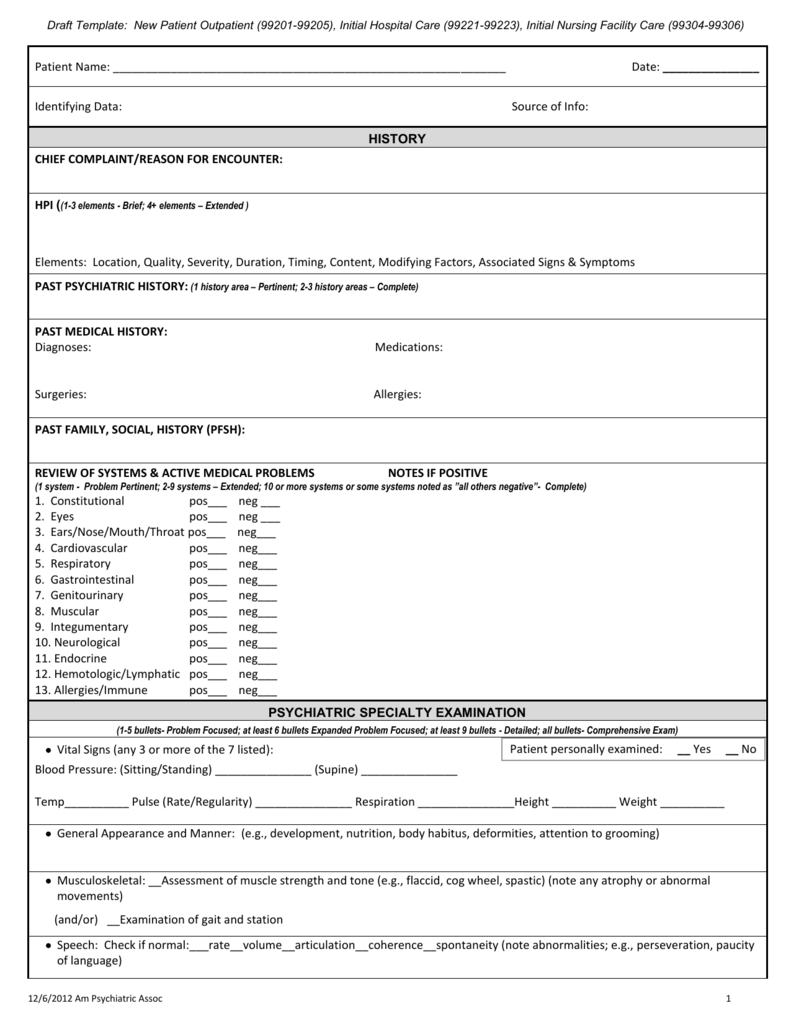
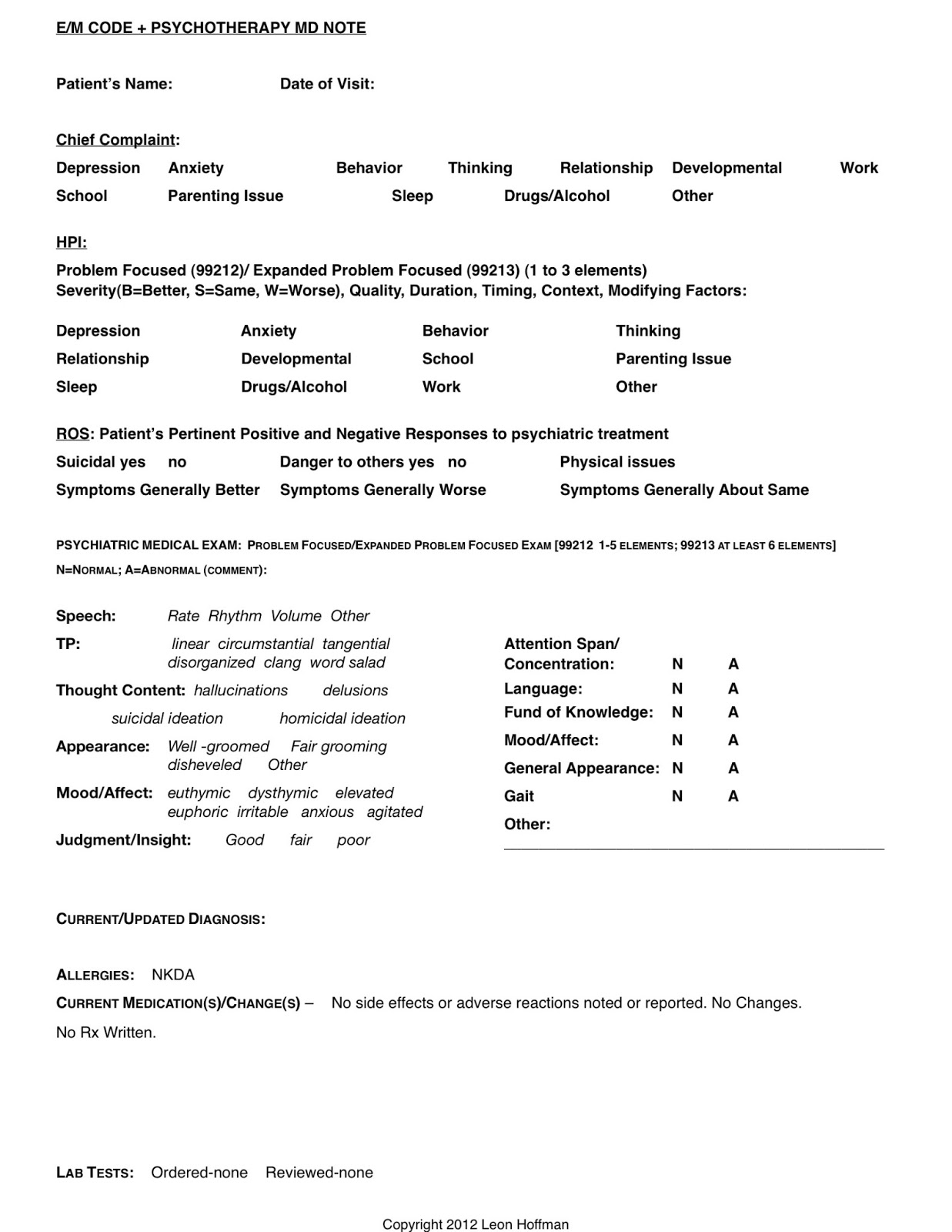
Psychiatry Hpi Template Master of Documents
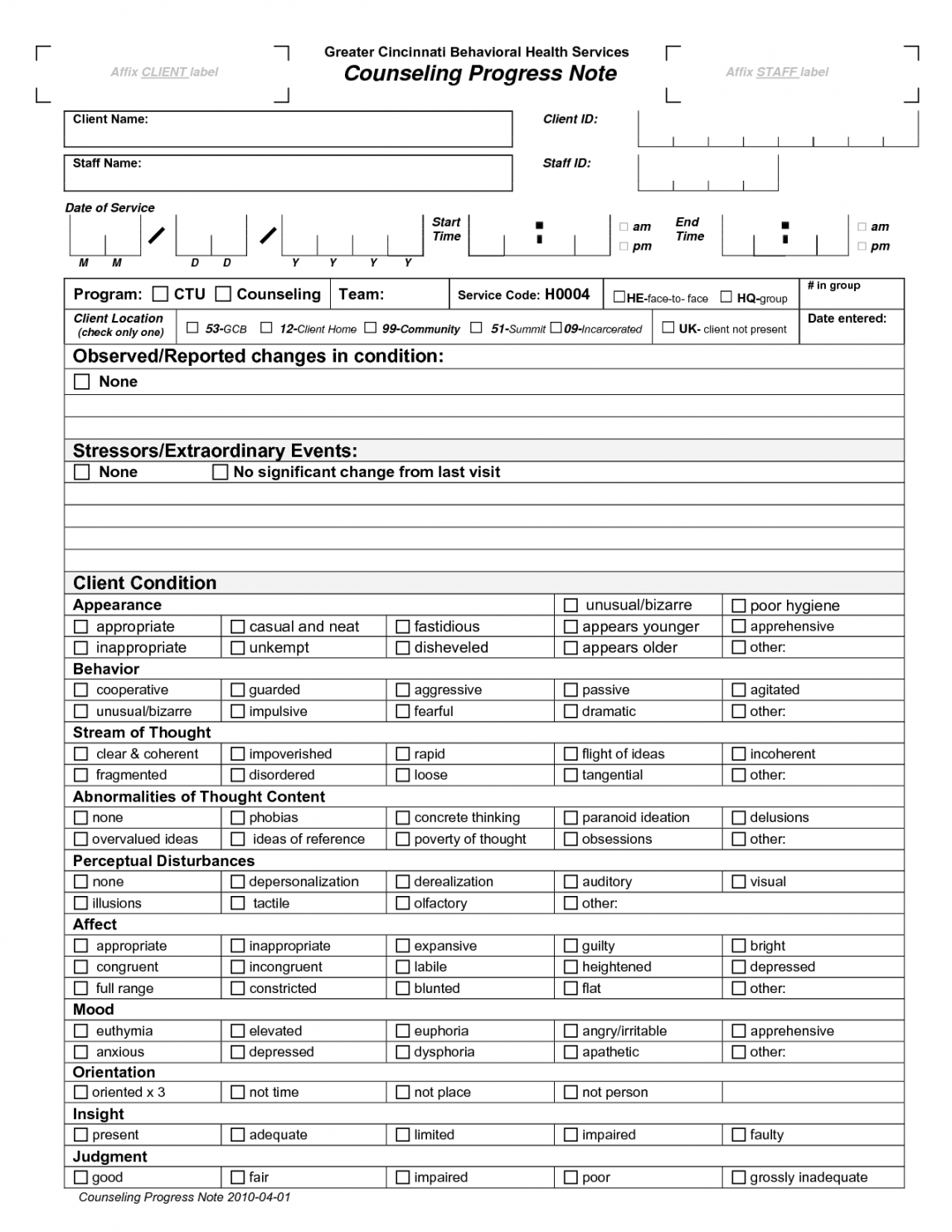
Editable Pin En Terapia Psychiatric Progress Note Template PDF IDTcenter
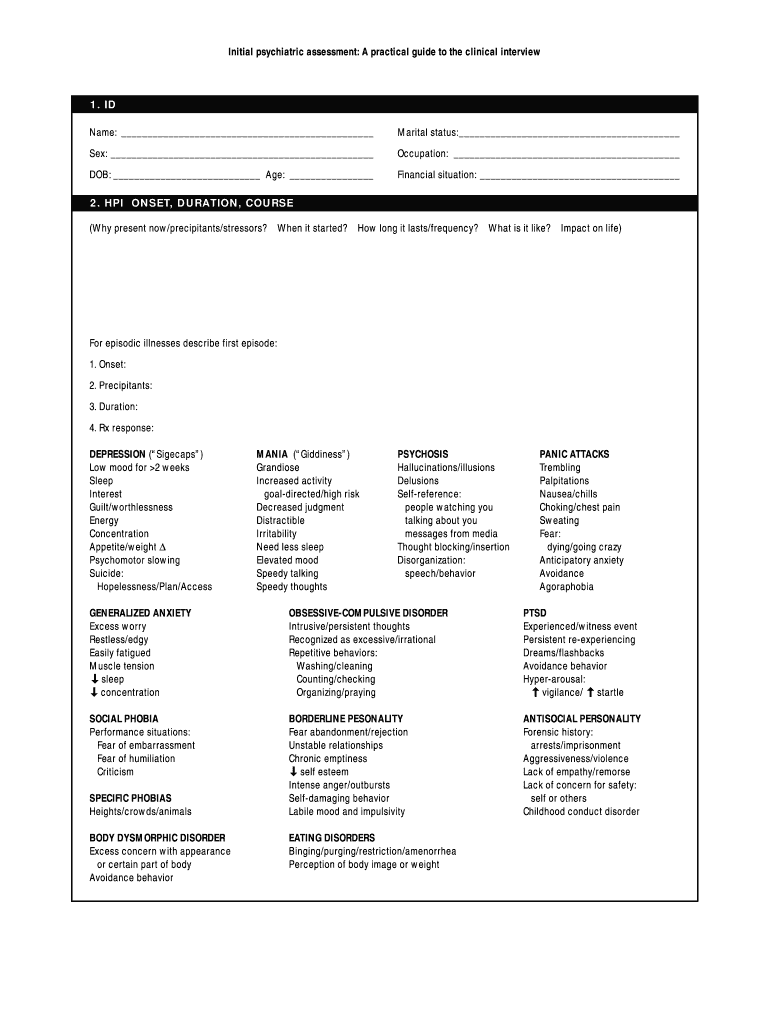
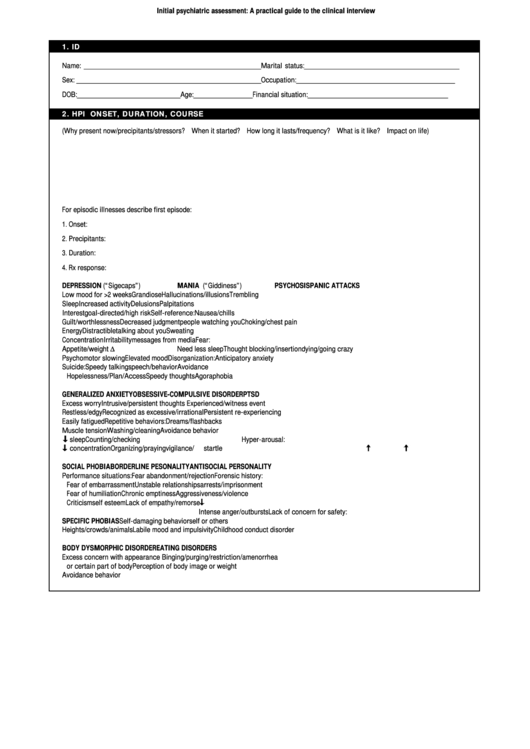
Psychiatric Assessment Guide Fill Online, Printable, Fillable, Blank
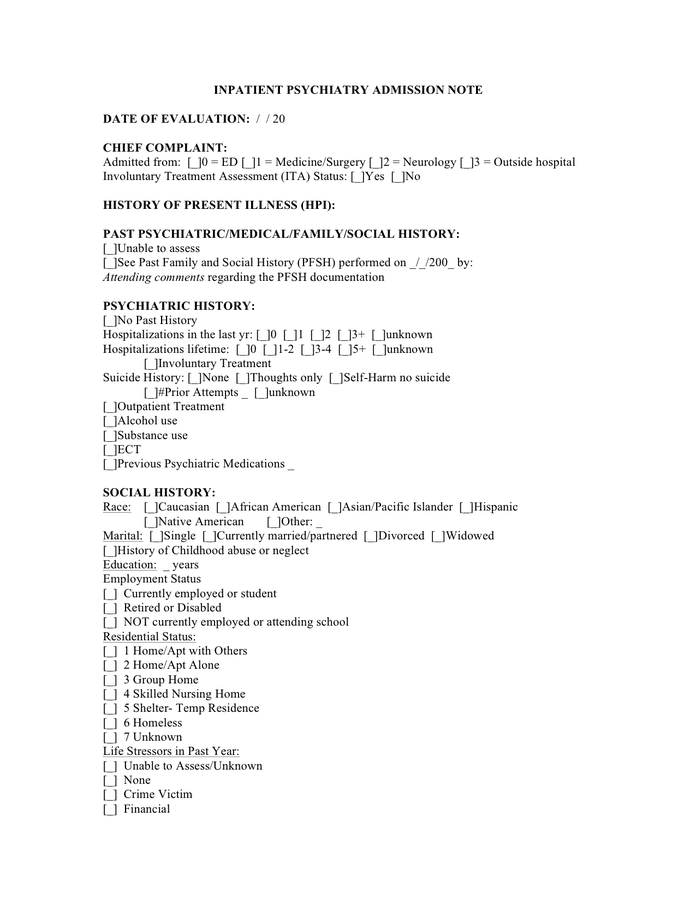
Inpatient psychiatric admission note in Word and Pdf formats
Psychiatry Hpi Template Master of Documents
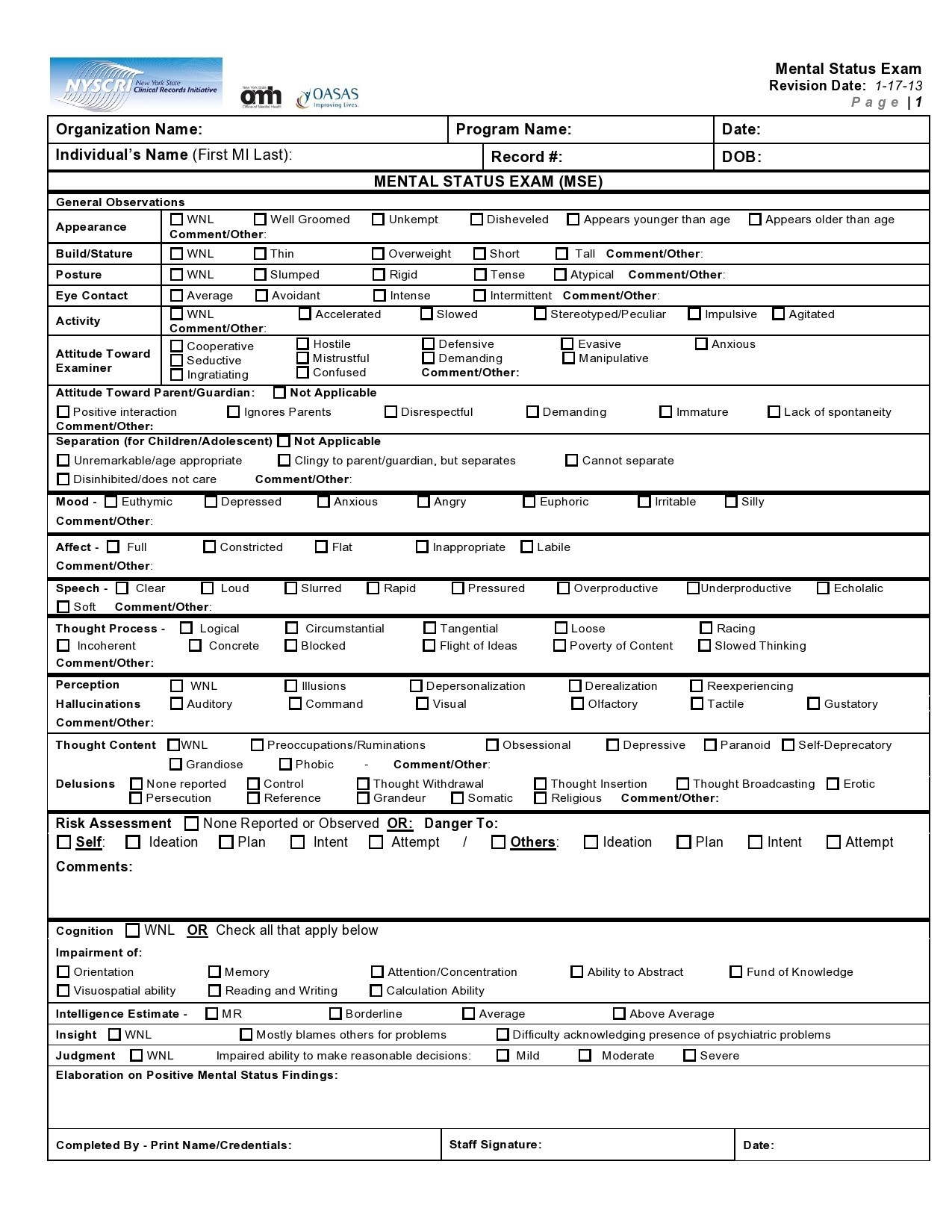
47 plantillas gratuitas de exámenes de estado mental (ejemplos de MSE
PROGRESS NOTE Counseling Worksheets, Therapy Worksheets, Counseling
Printable H&p Template Printable Word Searches
Top 5 Psychiatric Evaluation Form Templates Free To Download In Pdf
Related Post: