Physical Exam Note Template
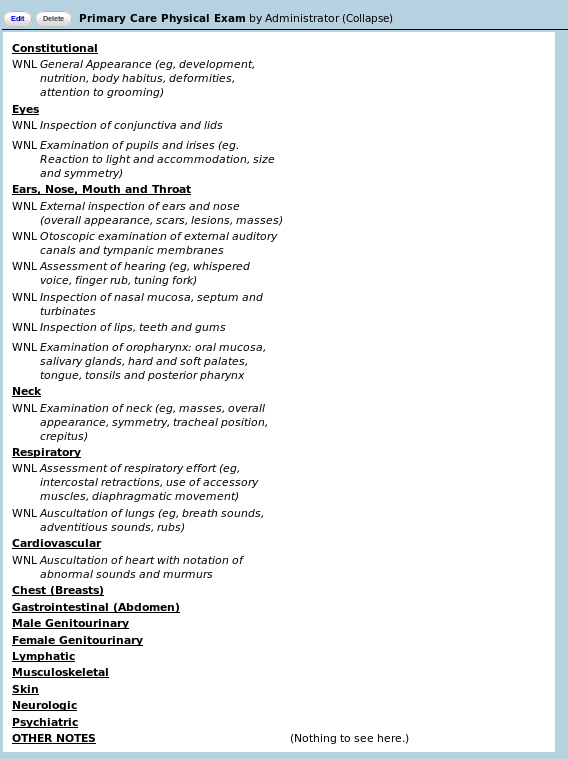
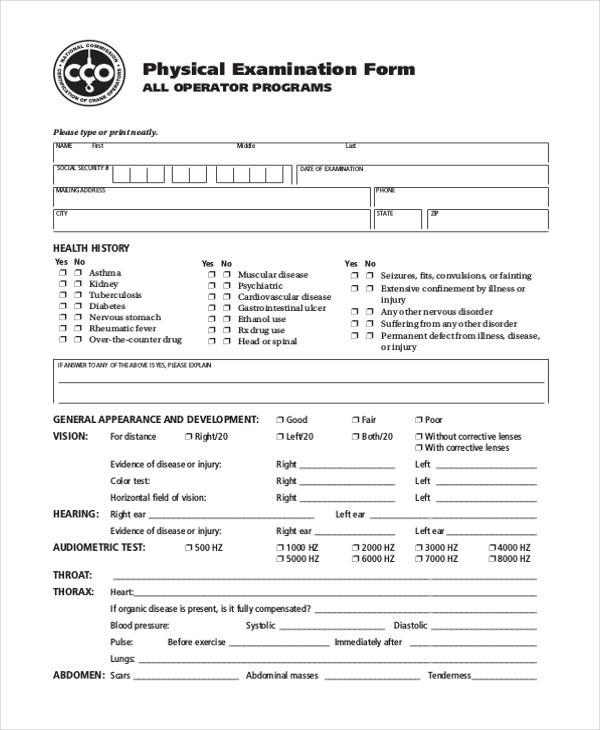
Physical Exam Note Template - Web soap notes format in emr soap stands for subjective, objective, assessment, and plan standard elements of soapnote date: Web physical note means any note in certificated form registered in the name of a holder other than dtc or its nominee. Most commonly used phrases in physical exam. Here are some guides and sample. No deformities or signs of scoliosis. Approximately 1,078 views in the last month. P / bp / rr / spo2 / t [1] i have reviewed the triage vital signs. The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Web sample template for normal comprehensive physical exam vital signs: Web the physical exam items can be completed quickly by circling “normal” or “abnormal” and noting any specific abnormalities. No deformities or signs of scoliosis. Subjective physical exam understand that the physical. Approximately 1,078 views in the last month. Web sample template for normal comprehensive physical exam vital signs: Web so here is a physical exam template that you can use in order to document a physical exam on a telemedicine visit. A neuro exam is one of the most complex to master when it comes to. Normal physical exam template description: Most commonly used phrases in physical exam. In the chart, the shaded. It allows for an initial assessment of. Web the guidelines include a detailed chart that specifies the exam elements that must be performed and documented to justify each level of exam. Web the physical exam items can be completed quickly by circling “normal” or “abnormal” and noting any specific abnormalities. “plan” has the meaning provided in section 4.02 (t). Soft, nt/nd, nbs, no masses or organomegaly. Approximately. Web free download physical exam templates. In the chart, the shaded. A&ox3, otherwise as per below. Well developed, well nourished, alert and cooperative, and. It allows for an initial assessment of. Web general adult physical exams. Below the exam items, space is also provided for. Web history and physical examination (h&p) examples. Web medical specialty:office notessample name: Normal external ears, normal tms. Web general adult physical exams. Web the guidelines include a detailed chart that specifies the exam elements that must be performed and documented to justify each level of exam. Here are some guides and sample. Well developed, well nourished, alert and cooperative, and. Web so here is a physical exam template that you can use in order to document a. A neuro exam is one of the most complex to master when it comes to. Web keep everyone in the loop by documenting exam findings and your next steps with the patient. Web the guidelines include a detailed chart that specifies the exam elements that must be performed and documented to justify each level of exam. Web so here is. Well developed, well nourished, alert and cooperative, and. In the chart, the shaded. Perrl, red reflex present bilaterally. P / bp / rr / spo2 / t [1] i have reviewed the triage vital signs. The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Approximately 1,078 views in the last month. Web free download physical exam templates. Web the guidelines include a detailed chart that specifies the exam elements that must be performed and documented to justify each level of exam. Web you are responsible for performing an appropriate physical exam and documentation for your patients. The physical examination is typically the first diagnostic. Here are some guides and sample. Below the exam items, space is also provided for. No deformities or signs of scoliosis. Most commonly used phrases in physical exam. No skin rashes or abnormal lesions. Web free download physical exam templates. “plan” has the meaning provided in section 4.02 (t). Web sample template for normal comprehensive physical exam vital signs: In the chart, the shaded. Subjective physical exam understand that the physical. A&ox3, otherwise as per below. Well developed, well nourished, alert and cooperative, and. Web you should always accompany an exam of the back and neck with an extremity, abdominal, neurological, respiratory, and cardiovascular exam, at least to some extent. Web history and physical examination (h&p) examples. Web the guidelines include a detailed chart that specifies the exam elements that must be performed and documented to justify each level of exam. Normal physical exam template description: Web the physical exam items can be completed quickly by circling “normal” or “abnormal” and noting any specific abnormalities. It allows for an initial assessment of. A neuro exam is one of the most complex to master when it comes to. Web soap notes format in emr soap stands for subjective, objective, assessment, and plan standard elements of soapnote date: Are you running out of ideas regarding what components your clinical exam should consist of? P / bp / rr / spo2 / t [1] i have reviewed the triage vital signs. The physical examination is typically the first diagnostic measure performed after taking the patient's history. (medical transcription sample report) eyes: Here are some guides and sample.8 Complete Physical Exam Template Template Monster
Printable Physical Exam forms Luxury Student Physical Examination form
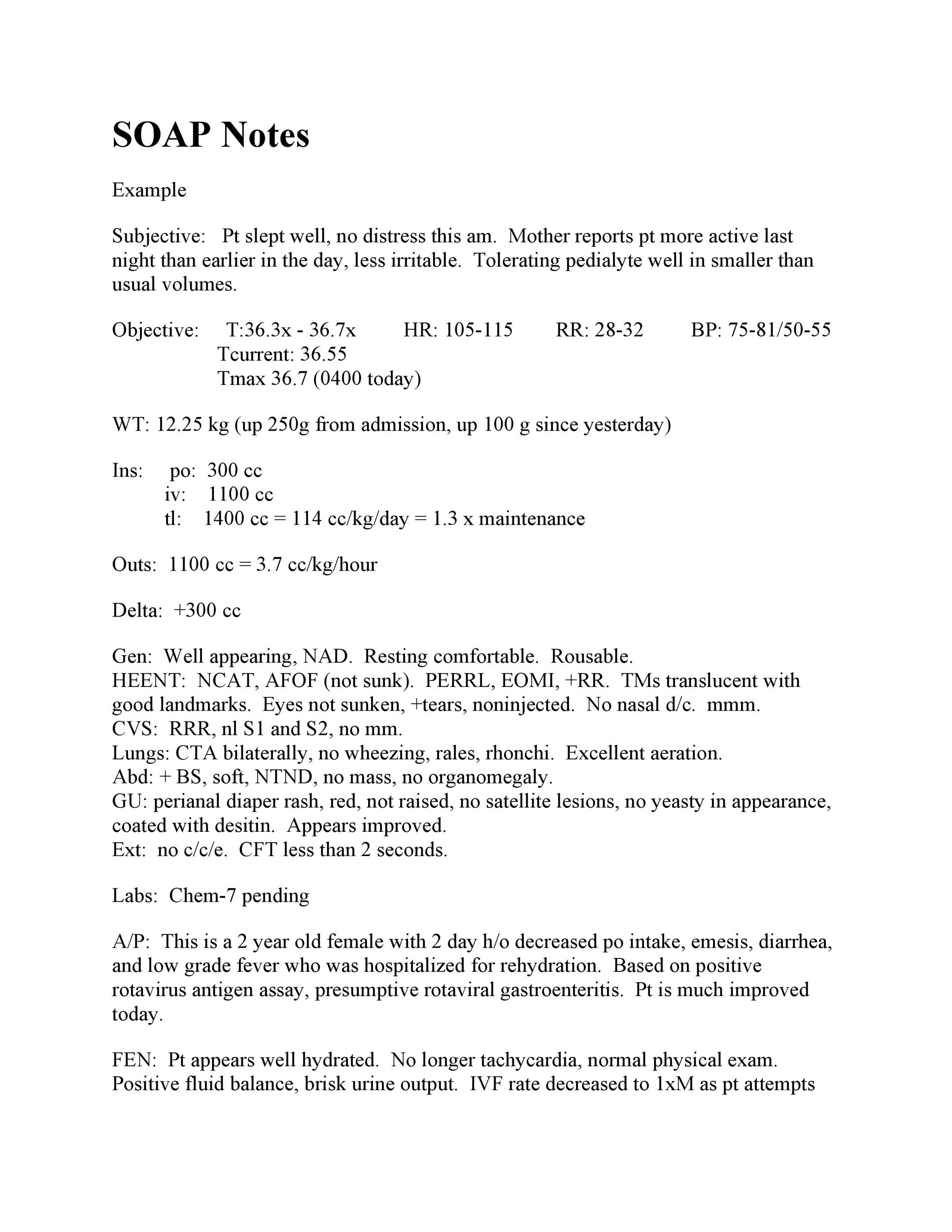
40 Fantastic SOAP Note Examples & Templates Template Lab
Daily Progress Notes Physical Examination Patient
Comprehensive Physical Exam Template Sample Templates
Physical Exam Template Check more at
the sample form for an animal research paper
Normal Physical Exam Template & Example Free PDF Download
Physical exam template in Word and Pdf formats page 2 of 2
43 Physical Exam Templates & Forms [Male / Female] Doctors note
Related Post:




.png)

![43 Physical Exam Templates & Forms [Male / Female] Doctors note](https://i.pinimg.com/736x/e1/da/2c/e1da2ce4b10a3fd7fa563ddbc571729e.jpg)