Outpatient Mental Health Discharge Summary Template
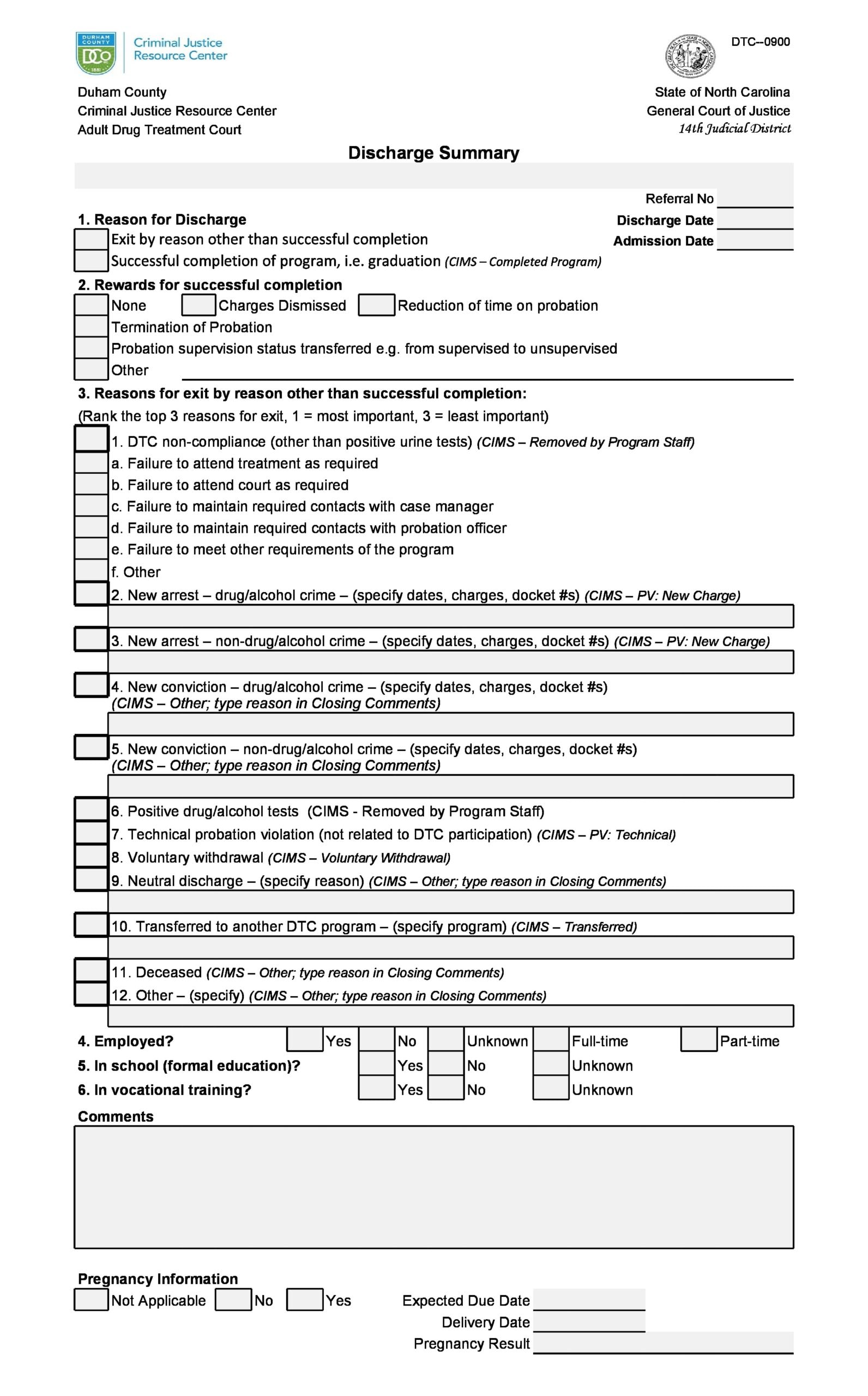
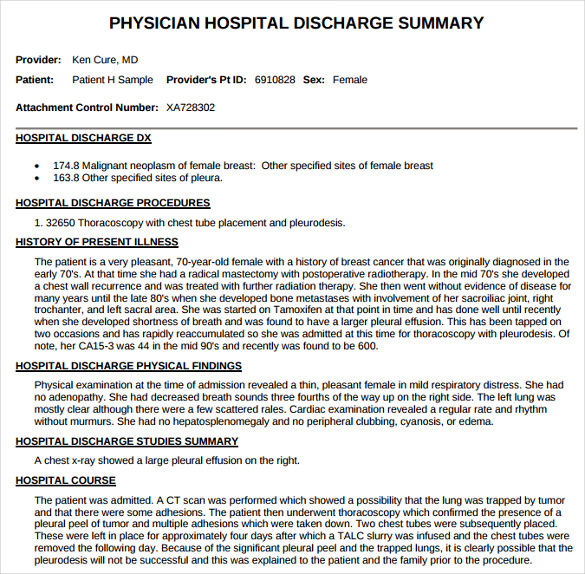
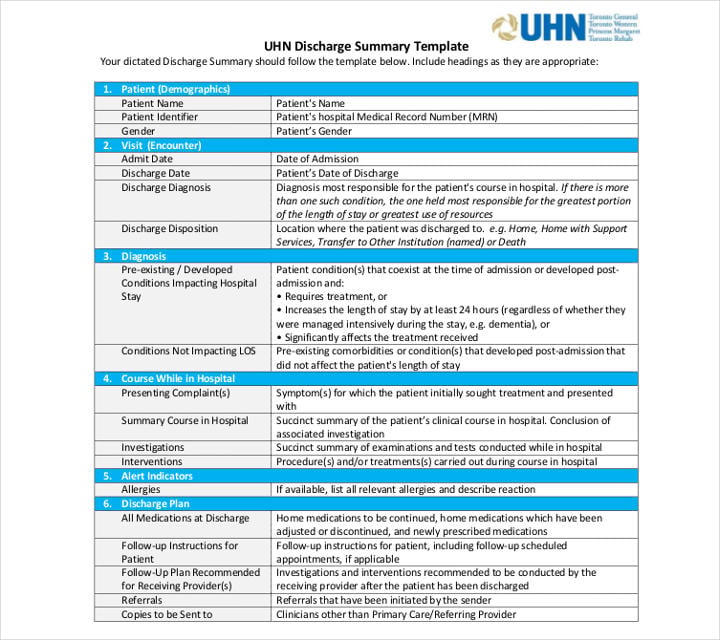
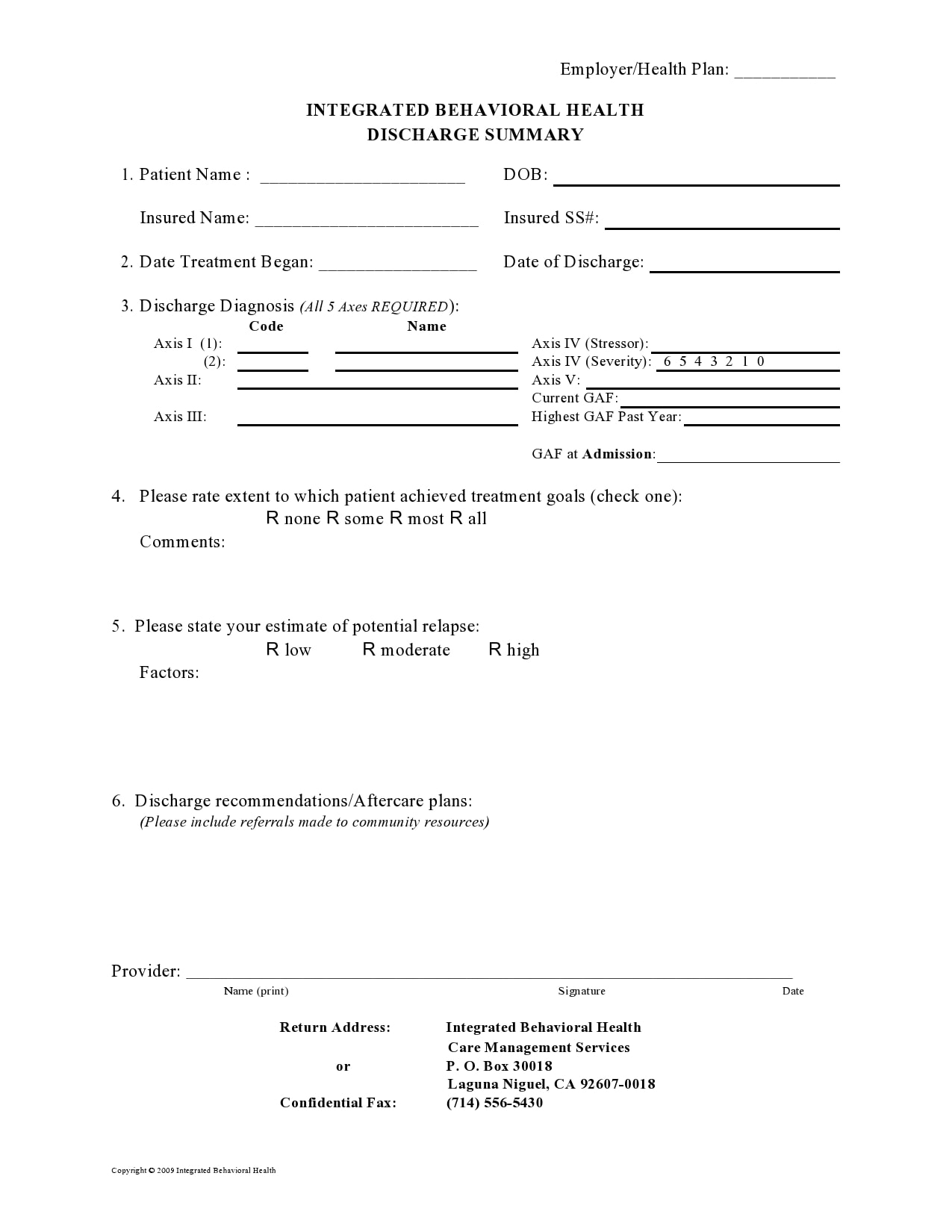
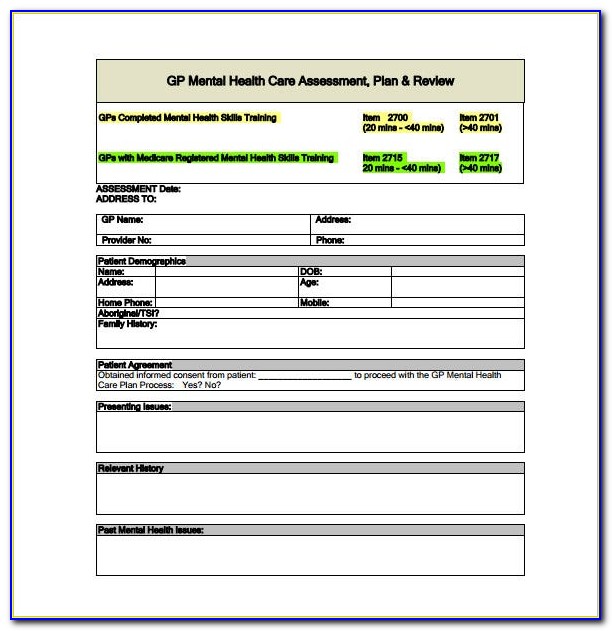
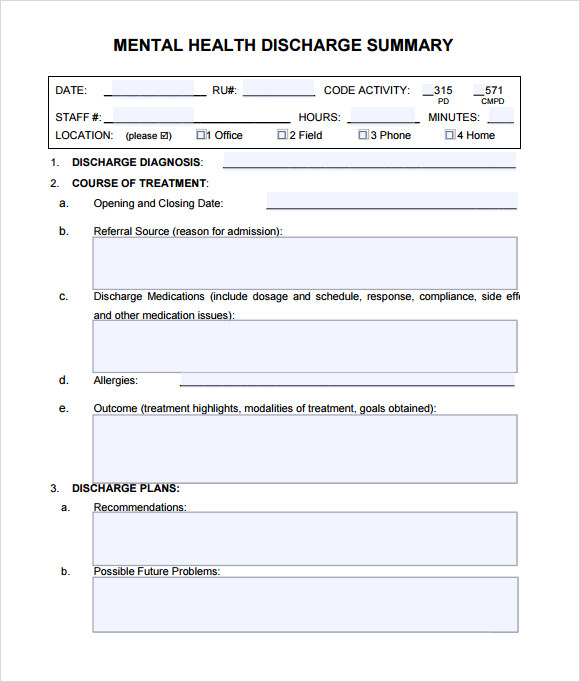
Outpatient Mental Health Discharge Summary Template - History and physical examination, medical clearance evaluation, psychiatric clearance as clinically indicated. John doe 10050049 2/15/1965 date admitted: A discharge note, also called a termination note, is a written summary held in the client’s chart of what happened during the time the client was in your care. Level of safety observation, as clinically. Web core functions of a discharge planner may include: Web sample discharge templates. Web the psychiatric discharge letter (or summary) typically serves two masters: Looking for mental health care providers? Web 1/1/2015 3:15 pm discharge plan patient name: Ad intake forms & documentation for mental health practitioners. Level of safety observation, as clinically. A progress note typically uses a soapor girpformat and documents weekly sessions. Ad intake forms & documentation for mental health practitioners. Web patient's diagnosis on admission: Prepare the necessary documentation, including a summary of the patient's stay, diagnoses, treatment. Soap notes are extremely helpful in counseling. A progress note typically uses a soapor girpformat and documents weekly sessions. Web a discharge summary is created when a patient’s case is closed and referred to another provider either by discharge from an inpatient or outpatient. History and physical examination, medical clearance evaluation, psychiatric clearance as clinically indicated. A discharge note, also called a. Level of safety observation, as clinically. A discharge note, also called a termination note, is a written summary held in the client’s chart of what happened during the time the client was in your care. Web patient's diagnosis on admission: An internal purpose is for future reference within secondary care, and the external purpose is to. If you or a. The patient’s diagnoses were not changed during the course of admission. A discharge note, also called a termination note, is a written summary held in the client’s chart of what happened during the time the client was in your care. Has never received outpatient mental health treatment. Level of safety observation, as clinically. Reference data classification category 1 patient i.d. Web 39 rows intake forms documents administrative forms [ help with pdf files ] the mental health division provides an array of opportunities for partners to work together in the. A progress note typically uses a soapor girpformat and documents weekly sessions. Level of safety observation, as clinically. Policies and procedures for services provided at or by an outpatient treatment center are. Web psychiatric discharge summary sample report #4. If you or a loved one have recently received treatment for a mental health condition, it can be overwhelming to navigate the discharge process. History and physical examination, medical clearance evaluation, psychiatric clearance as clinically indicated. Scheduling by inpatient psychiatric providers of outpatient appointments with mental health providers. Web this study examined a. Having an easy to use soap note like our editable pdf soap notes allow practitioners to easily store client and patient notes, organized by each session that they attend. Web this study examined a key discharge planning practice: An internal purpose is for future reference within secondary care, and the external purpose is to. Web soap notes help a private. Nesmith has a history of suicidal thoughts but has never. Scheduling by inpatient psychiatric providers of outpatient appointments with mental health providers. Policies and procedures for services provided at or by an outpatient treatment center are established, documented, and implemented to protect the health and safety of a patient. Web 1/1/2015 3:15 pm discharge plan patient name: Prepare the necessary. Nesmith has a history of suicidal thoughts but has never. Initiate bh disposition pathway order set. Web 39 rows intake forms documents administrative forms [ help with pdf files ] the mental health division provides an array of opportunities for partners to work together in the. Soap notes are extremely helpful in counseling. Level of safety observation, as clinically. Additionally, as a resource for sondermind providers, we’ve created a discharge template that you can access here. Soap notes are extremely helpful in counseling. Web patient's diagnosis on admission: Level of safety observation, as clinically. Suicide prevention bundle, as clinically indicated. Web 1/1/2015 3:15 pm discharge plan patient name: Has never received outpatient mental health treatment. Ad intake forms & documentation for mental health practitioners. Web sample discharge templates. Prepare the necessary documentation, including a summary of the patient's stay, diagnoses, treatment. John doe 10050049 2/15/1965 date admitted: Reference data classification category 1 patient i.d. A discharge note, on the other hand, spans a broader amount of. Web inpatient who may require behavioral health (bh) discharge disposition. Scheduling by inpatient psychiatric providers of outpatient appointments with mental health providers. Suicide prevention bundle, as clinically indicated. Having an easy to use soap note like our editable pdf soap notes allow practitioners to easily store client and patient notes, organized by each session that they attend. Web patient's diagnosis on admission: Soap notes are extremely helpful in counseling. Initiate bh disposition pathway order set. An internal purpose is for future reference within secondary care, and the external purpose is to. Intuitive intake forms, scheduling, billing, telehealth & more The patient’s diagnoses were not changed during the course of admission. If you or a loved one have recently received treatment for a mental health condition, it can be overwhelming to navigate the discharge process. (name, doc#, dob) behavioral health discharge summary date of summary current facility unit (optional) date entered doc erd/prd 1.6+ Discharge Summary Template Free PDF, Word, Excel Formats
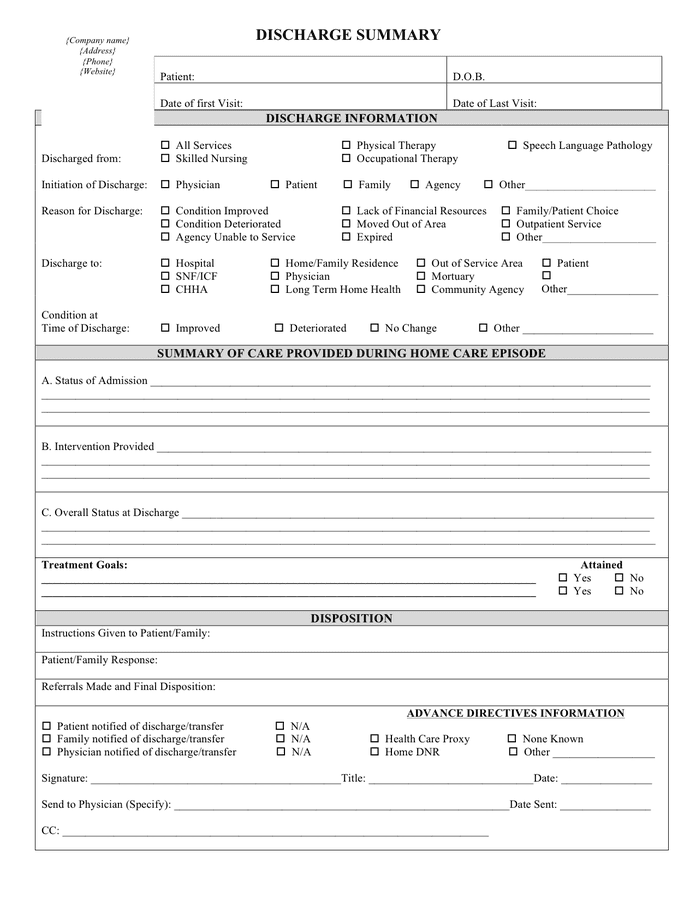
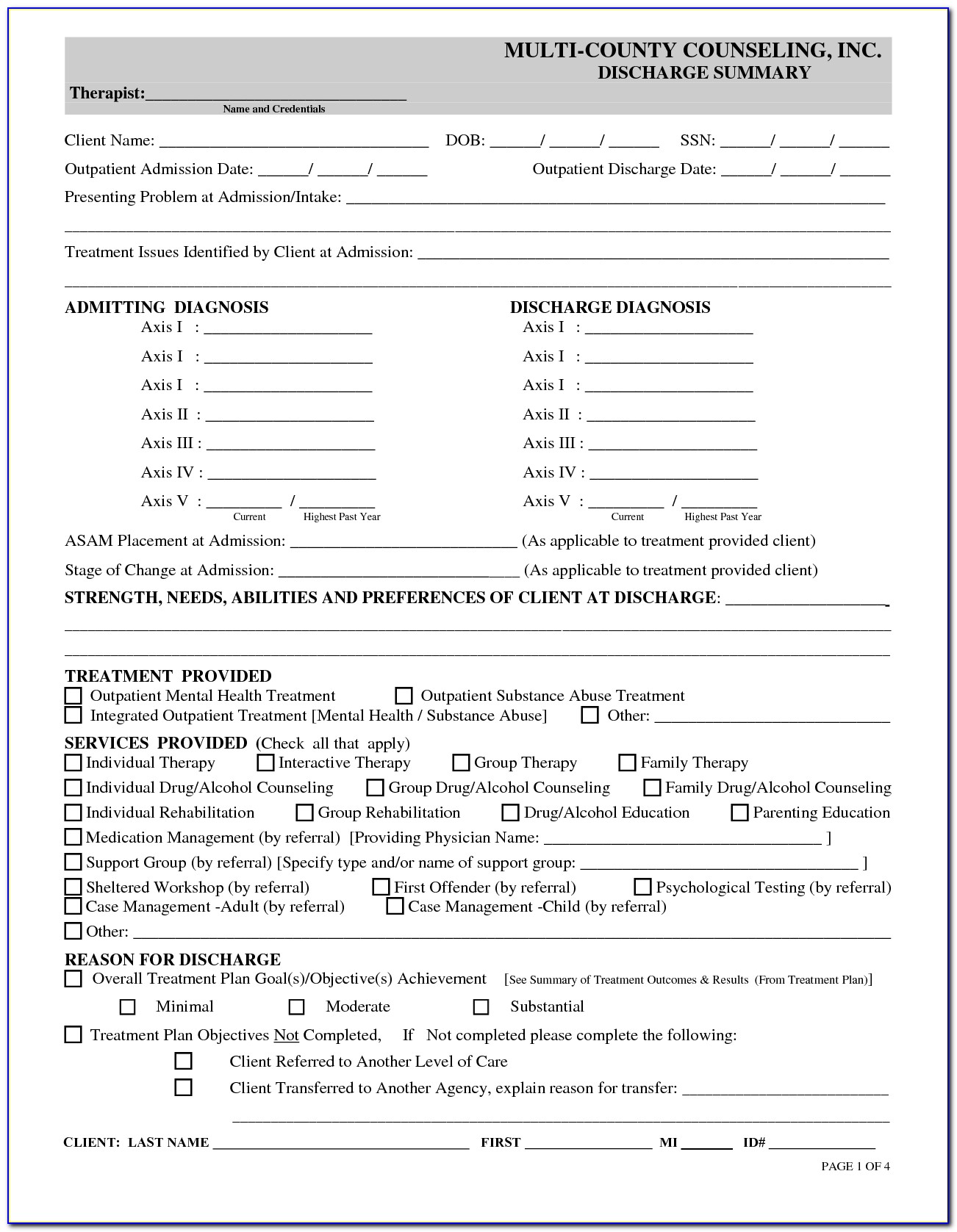
Discharge summary template in Word and Pdf formats
Outpatient Mental Health Discharge Summary Template
30 Hospital Discharge Summary Templates (& Examples)
FREE 14+ Sample Discharge Summary Templates in MS Word PDF
10+ Discharge Summary Templates PDF, DOC
30 Hospital Discharge Summary Templates (& Examples)
Mental Health Treatment Plan Template Pdf
FREE 7+ Sample Discharge Summary Templates in PDF MS Word
30 Hospital Discharge Summary Templates (& Examples) Behavioral
Related Post: